MEDI-CAL
MANAGED CARE

What Is Medi-Cal Managed Care?
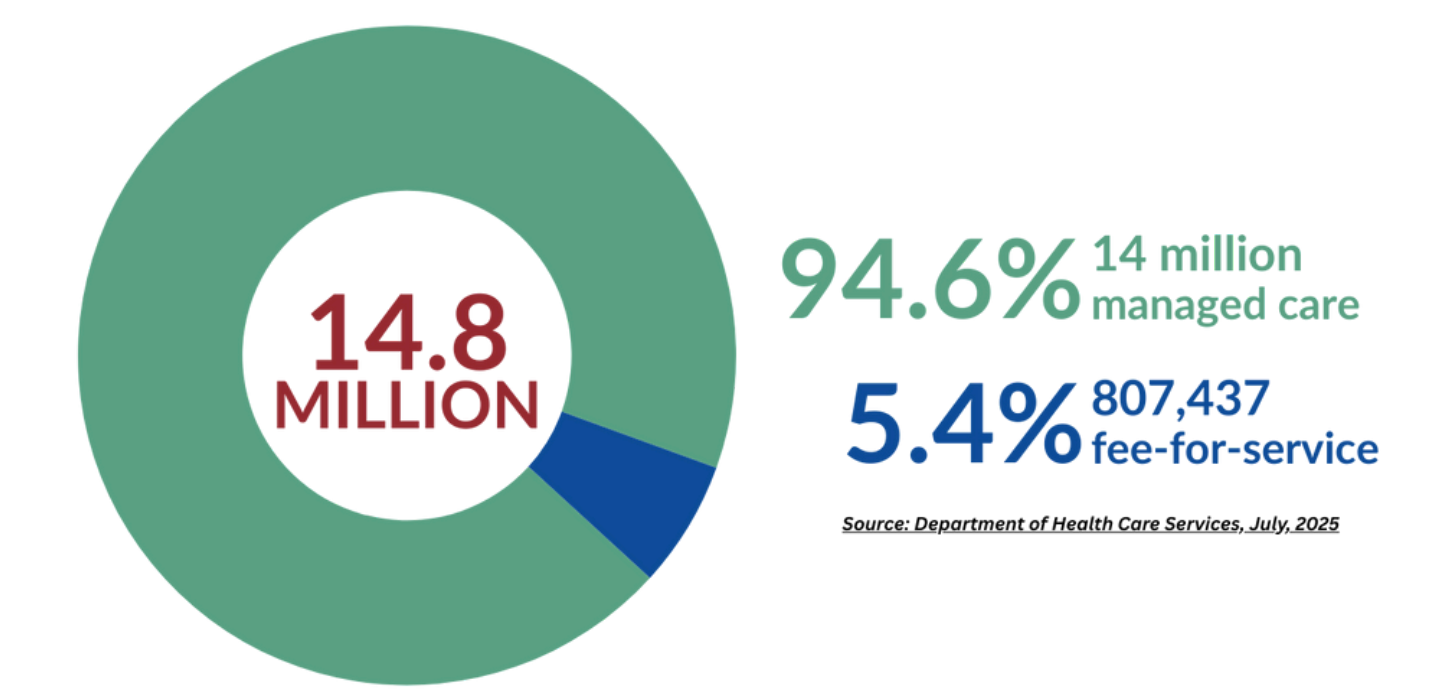
Medi-Cal Managed Care is the foundation of California’s Medi-Cal system, serving more than 14 million people. Medi-Cal managed care plans provide more than doctor visits — they deliver whole-person, community-based coverage that supports physical and behavioral health, maternal and child wellness, housing stability, nutrition, and more.
By addressing both medical and social needs, Medi-Cal managed care helps Californians stay healthy, avoid medical debt, and live with dignity. It’s a lifeline for children, families, seniors, people with disabilities, and workers across all 58 counties.
Estimated Medi-Cal Enrollment
Low-income Children and Families

Pregnant Individuals

Childless Adults
Seniors and Persons with Disabilities

Medi-Cal Managed Care helps vulnerable communities
1 in 3
16.7%
40%
36.5%

Coverage Options in all California Counties
Medi-Cal Managed Care is available in all 58 counties, including rural areas.
Counties follow one of several models – county organized health systems, geographic managed care (GMC), two-plan, regional, and models specific to Imperial and San Benito counties.
Medi-Cal Managed Care: Services Snapshot
Full Scope Medi-Cal Coverage
- Prescribed medications
- Doctor visits
- Vaccines
- Mental health care
- Substance use care
- Vision care/eyeglasses
- Referrals to specialists
- Dental care
- Hearing aids
- Appointment Transportation
- In-home care
- Long-term care
- Emergency services
- Much more

Enhanced Care Management and Community Supports
Medi-Cal Managed Care plans are addressing the social drivers of health—like housing and nutrition—that help people stay healthy and avoid chronic illness. This includes critical support for older adults and in-home services that help people live independently.
Enhanced Care Management
Enhanced Care Management (ECM) is a statewide Medi-Cal managed care plan (MCP) benefit that provides equitable, person-centered, and community-based care management for members with complex needs.
Enrolled members receive comprehensive care management from a single lead care manager who coordinates all their health and health-related care, including physical, mental, and social services.
The lead care manager meets them wherever they are — on the street, in a shelter, in their doctor’s office, or at home.

Community Supports
Community Supports address MCP members’ social drivers of health and helps them avoid higher, costlier levels of care.
The Department of Health Care (DHCS) has preapproved 15 services that MCPs are encouraged to offer as Community Supports, which include:

Housing Transition Navigation Services
Housing Deposits

Transitional Rent
Short-Term Post-Hospitalization Housing
Day Habilitation Services

Recuperative Care (Medical Respite)
Housing Tenancy and Sustaining Services
Asthma Remediation

Respite Services
Nursing Facility/ Assisted Living Facility Transitions
Community or Home Transition Services
Personal Care and Homemaker Services
Medically Tailored Meals

Sobering Centers
Environmental Accessibility Adaptations
Medi-Cal Managed Care Enjoys Broad Support
There is widespread support amongst all demographics that we should protect the progress we have made over the last decade.
↑ 90%
↑ 70%
Many Californians have personal or family experience with Medi-Cal. Over half of Californians responded that Medi-Cal was important to them and their families.
Medi-Cal Managed Care Oversight
Department of Health Care Services - Medi-Cal Administration
Department of Managed Health Care - Medi-Cal Managed Care Regulation
Medi-Cal Rates: